It starts with a queasy feeling, then nausea, then quickly progresses to several hours of vomiting and diarrhea. It’s difficult to keep down anything at all, which brings on the headache and dizziness of dehydration. Many of us have been there, victims of the ubiquitous stomach bug. It may surprise you that a Stomach Bug is not a single illness but many viruses and bacteria that can cause similar symptoms. One of the most common causes is Norovirus, a viral infection that spreads quickly from person to person. Another potential cause of a Stomach Bug is the bacteria Shigella sonnei.
Norovirus
Norovirus begins and ends in humans. We are the only “reservoir” for Norovirus, meaning that this virus comes only from humans. Norovirus is highly contagious, spreading through feces between humans on contaminated surfaces, foods, water, and even the air in a recently used restroom. Norovirus does not have the protein envelope we see in flu or COVID, making it more durable in the environment. Alcohol-based hand sanitizers do not destroy it. According to the Centers for Disease Control and Prevention (CDC), the most common variant of Norovirus responsible for recent outbreaks worldwide is the GII.4 genotype. While the world focused heavily on COVID and transmission prevention for the past few years, we saw a decline in all contagious viral infections. A February 2023 article in TIME Magazine discusses an expected rise in our seasonal illnesses as COVID-19 social distancing, mask-wearing, and isolation practices fall by the wayside. The article focuses on recent upticks in Norovirus infection. They report that in January of this year, the Norovirus Sentinel Testing and Tracking network (NoroSTAT) saw an increase in national outbreaks from 15 to 26. By early February, the National Respiratory and Enteric Virus Surveillance System (NREVSS) reported an increase in the U.S.’s three-week average of positive Norovirus tests from 10.5% to 15%. Last week, local news sources said that over 100 school-aged children in a single Phoenix, AZ neighborhood experienced illness associated with a local norovirus outbreak.
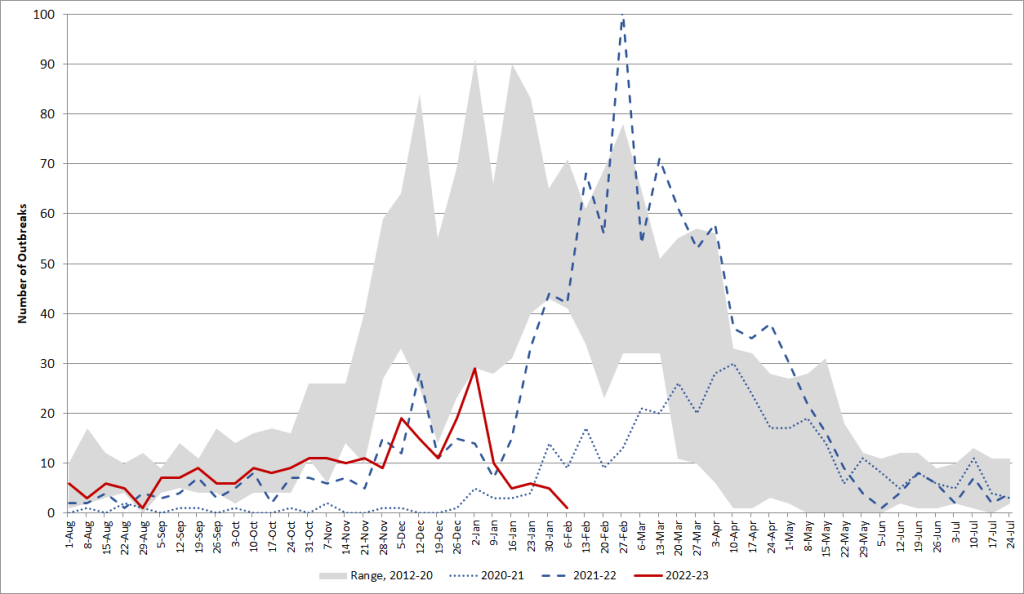

Norovirus outbreaks are not limited to the United States. Last April, the Public Health Agency of Canada posted a notice alerting Canadians to a nationwide Norovirus outbreak traced to contaminated oysters from British Columbia. Local infectious disease experts remarked that Norovirus is transmitted through feces, and the virus can survive for long periods in sewage systems. They share that outlets from sewers into water sources regularly test positive for Norovirus. Later, in December of 2022, the United States saw its own oyster-spread norovirus outbreak. The FDA reported that oysters harvested from Texas late last year caused illness throughout the south, in states including North Carolina. As countries continue to lift their travel restrictions, remote countries like the small pacific archipelago republic of Palau see an increase in infectious illness, including a February 2023 Norovirus outbreak. Most notably, government health agencies in England are reporting significantly increased trends in norovirus cases. In an update just last week, the U.K. Health Security Agency reported positive norovirus testing at rates “more than double the 5-season average prior to the coronavirus (COVID-19) pandemic.” Many cases are associated with nursing homes and assisted living facilities in people over 65. The dehydration and electrolyte imbalance associated with Norovirus impact elderly individuals and very young children more severely. Facilities where people cannot fully isolate when sick, such as nursing homes and college dormitories, are especially susceptible to infectious illness, and Norovirus is no exception. The chief executive of Care England, a British non-profit organization that assists seniors, shares with local news that underfunding facilities and short staffing may contribute to the current outbreak.
Shigella sonnei
Another relatively common cause of Stomach Bugs is the bacteria from the genus Shigella. We often see infections with the Shigella sonnei bacteria in the United States. In recent months, public health organizations across multiple countries have seen a concerning rise in Shigella sonnei infections. Most alarmingly, U.S. news outlets write that the Shigella sonnei strain associated with this current outbreak is highly resistant to antibiotics. The CDC’s emergency bulletin from late last month reports that the number of “extensively drug-resistant” or “XDR” Shigella sonnei infections increased from 0% in 2015 to 5% in 2022. The CDC shares that it does not currently have a recommended course of treatment for this S. sonnei infection as the bacteria has proven resistant to standard and last-resort antibiotic treatments. The CDC’s primary concern is that the bacteria can share their antibiotic-resistant genes with other related bacteria, which could produce even more extensively drug-resistant infections. Like Norovirus, Shigella lives only in humans and spreads when we swallow infected feces. Unfortunately, we need only consume a microscopic amount of fecal material before becoming infected.

The European Centre for Disease Prevention and Control (EDCD) has tracked this outbreak closely and found a common thread: travelers returning from Sal, Cabo Verde. The EDCD’s case-reporting system captured 258 S. sonnei infections associated with travelers from Cabo Verde (221 confirmed, 37 suspected). Epidemiologists and genome sequencing have zeroed in on all-inclusive hotels in the southern Santa Maria region of Sal. The EDCD warns of associated cases as recent as January of this year and the potential for ongoing infection in travelers to that area. The EDCD is clear that with this specific outbreak, they have yet to identify a common exposure. They state that the most likely cause is foodborne transmission through infected handlers. Still, some cases may be due to person-to-person transmission. Men who have sex with men may be at an increased risk of developing S. sonnei infection. Sexually-associated infections can carry a significant stigma. It is crucial to clarify that the current data show more infections in women than men (2.5:1). Other common at-risk groups for S. sonnei infection include children and individuals living closely with others.
So what?
So what can we do about it? Many pathogens that cause the symptoms we associate with a Stomach Bug come from oral contact with infected feces. Handwashing with soap and water continues to be critical in breaking the chain of transmission for these diseases. Stay home if you’re not feeling well, especially if you handle food. And if you do find yourself rushing to the bathroom one of these days, stay hydrated with plenty of fluids and electrolytes.
